What are warts? We will analyze the causes, diagnosis and treatment methods in an article by a dermatologist with 37 years of experience.

Definition of disease. Causes of disease
Wartsare mild, irregular, benign skin lesions in the form of localized overgrowths of the top layer of skin (epidermis) with papules (nodules) or plaques.
The incidence of warts in adults is 7-12%, in school-aged children - up to 10-20%.
Warts are very similar to other skin growths. Usually a person cannot accurately determine the disease by himself, so he must consult a dermatologist to make a diagnosis.
Human papillomavirus is the cause of warts. The type of virus affects the types of warts that can develop. Thus, each type of human papillomavirus infects the tissue at its most characteristic location.
| HPV type | Preferably |
localizationTypes of warts |
|---|---|---|
| 1 | feet, knees, palms, hands, fingers |
Plantar and palmar warts, rare simple warts |
| 2, 4 | Hands, fingers, knees, less frequently - feet |
Simple warts, sometimes plantar, palmar and mosaic warts |
| 3, 10 | Shins, hands, face | Flat warts |
| 7 | Hands, fingers | Butcher Warts |
| 5, 8, 9, 12, 14, 15, 17, 19-24 |
Face, arms, torso |
Epidermodysplasia verruciform |
Viral infection usually occurs through contact - by direct contact between infected skin and healthy skin (for example, when shaking hands) or indirectly (through handrails, toys, etc. ). Therefore, you can become infected with the human papillomavirus, which causes warts, in various places - on public transportation, at school, at work, at home, in places with high contact and humid environments (swimming pools, saunas, gyms. ). Minor trauma to the epidermis, through which the virus enters, as well as inflammation of the skin, contribute to infection.
Also contributes to the appearance of warts:
- immunodeficiency (including HIV infection);
- warm and humid environment;
- the need for professional contact with meat and fish ("butcher's warts").
Several types of human papillomavirus are transmitted from parents.
But toads and frogs, despite the horror stories that often scare us in childhood, cannot be infected - this is one of the most popular myths about this disease, which is unfounded.
If you find similar symptoms, consult your doctor. Don't self-medicate - it's dangerous to your health!
Symptoms of the wart
Symptoms will vary depending on the type of wart.

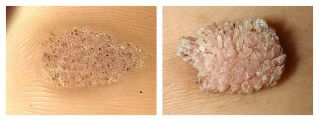
Common warts:
- Round solid papules of normal color, 1-10 mm and larger.
- Papule surface covered with cracks, layers.
- If the papule is on the finger, the printout disappears and becomes distorted. The same is true for palm images.
- Simple warts are located individually or in sections - usually appearing in the sites of greatest injury (hands, fingers, knees).
- When examined with a dermatoscope, the doctor may see tiny brown dots - blocked (clogged) capillaries. Patients often refer to these points as "roots". This is the main sign for a doctor: it can be used by a dermatologist to distinguish warts from other similar diseases (for example, molluscum contagiosum and keratoma).
Plantar (horny) warts:
- The main symptom that usually causes a patient to see a doctor is pain when pressing and walking.
- Such warts are usually localized on the legs.
- When contacting a doctor, usually, keratinized and uneven plaques of normal color are seen, although in the first stage you can see flat, smooth papules. With keratinization, capillaries can only be seen if the keratin layer of the skin is removed.
- The leather of the shoe sole is distorted.
- Plantar warts are usually solitary, but there are also 2-6 warts;
- These warts are often confused with corns (especially dry ones) - this is a description of the problem patients typically encounter.

Flat warts (teenagers):
- Looks like round, clear, smooth papules of normal color, pink or brownish, 1-5 mm in size.
- It appears on the hands, shins, very often on the face.
- There are always multiple warts - they are in groups.
Epidermodysplasia verruciform (senile wart):
- Large, round, multiple confluent neoplasms of normal color, pink or brown.
- Most commonly appears on the face, arms, front of the torso.
- May be confused with keratoma, shingles and skin cancer.
Pathogenesis of warts
Upon entering the body, the human papillomavirus can remain in a latent state for a long time - a person usually doesn't even notice its existence. When a favorable factor for virus emerges, it begins to "multiply" in the epithelium, causing tissue changes.
Unlike other viruses, human papillomavirus do not destroy epithelial cells themselves - they die by themselves, naturally, in the process of keratinization and exfoliation.
Local factors and the state of the immune system influence the spread of infection. For example, people with HIV infection or a kidney transplant are more likely to develop warts. In addition, these neoplasms are often difficult to treat. With normal immunity, the virus does not affect the deep layers of the skin, so many people get warts themselves after a few months.
The main stage of the appearance of warts is the acceleration of the rate of cell division and growth with the help of viruses. This rapid metabolism causes thickening of the skin layer. As the tissue grows in a certain small area, tubercles appear, which are called warts.
Classification and stages of development of
wartsThere is no generally accepted classification of warts. However, there are some common variations:
- Common wartsare the most common type (70% of warts are just warts). Such neoplasms are not felt and only cause aesthetic discomfort to a person.
- Plantar wart- appears on the soles of the feet, is painful, and therefore requires treatment. Skin trauma due to uncomfortable, tight, and abrasive shoes contributes to the development of such warts.
- Flat warts- more common in young people, adolescents. This is due to the unstable hormonal background of young people, which affects the whole body. Usually flat warts are barely visible.
- Senile warts- typical of older people. They often appear on parts of the body that are covered with clothing, but can appear on the face and hands. If there is no discomfort, such warts should not be treated - healing in the elderly can be much slower than in younger people, due to a slow metabolism.
Other authors distinguish several of these types of warts:
- Mosaic warts(HPV 2, 4) - neoplasms on the palms and soles of the feet. They look like a focus of hyperkeratosis, that is, thickening of the stratum corneum (usually in the forefoot), covered with deep cracks.
- Cystic warts(HPV 60) is a very rare type of neoplasm on the feet. This is a soft knot with cracks. Once opened, a white-yellow liquid, similar to curd.
- Filiform wartsare growths of thin horns near the mouth, nose or eyes.
- "Butcher" Warts(HPV 7) - appear on the hands and fingers of people who are in constant contact with meat and fish. Presented as a hypertrophic neoplasm similar to cauliflower, but normal in color.
Also, the types of warts differ depending on their location.
So, anogenital warts - tumor-like neoplasms that appear on the genitals (especially where the skin to mucous membrane transitions) is a common disease. Usually caused by HPV types 6 and 11.
Complications of warts
The main reason wart patients go to the doctor is aesthetic defects that can affect the patient's quality of life, self-confidence and develop a lot of complexity. Complications can also include surface rupture of the wart and increased infection, and in some types of warts, pain when walking.
Skin warts do not usually degenerate into malignant neoplasms, they are quite harmless, however, in very rare cases, such complications can still occur in people with a suppressed immune system.
Another complication arises when trying to remove a neoplasm on its own. In this case, inflammation and aesthetic defects in the form of scars can occur, as well as further spread of the virus through the skin, therefore, in the morning after self-removal of one wart, a person can wake up with several new warts.
Remember that under the guise of warts, a completely different disease can be hidden, which cannot be determined without the advice of an experienced doctor.

Diagnosis of
wartsUsually the examination (clinical picture) and history (medical history) are sufficient to make a diagnosis.
To confirm the diagnosis, the doctor can perform a histological examination - studying the neoplasm cells.
It is very important to make a differential diagnosis - to differentiate warts from other diseases. For example,common wartsmust be distinguished from the following diseases:
- Molluscum contagiosum- appears more frequently on the body and genitals, less frequently on the hands and feet. This is a hemisphere with an impression on the surface; when pressed from the side, a whitish "pulp" is released.
- Epidermal verrucous nevus- often solitary, a person is born. It rises above the surface of the skin, often covered in hair.
- Basalioma- a tumor in the form of a nodule roll, covered with a crust in the middle. Typical for parents.
Palmar-plantar wartsmust be distinguished from the following diseases:
- Keratoderma- large areas of keratinization and skin inflammation. No capillaries freeze.
- Palmar-plantar syphilides- multiple neoplasms without pain, peeling skin along the edges. Syphilis has a positive reaction
- Corn- usually painless, can only cause pain when pressed vertically.
Doctors must also distinguish other types of warts from a number of diseases. If another pathology is suspected, he may prescribe an additional diagnosis (for example, detection of antibodies to the virus, CT or MRI).
Wart treatment
Warts are treated for aesthetic purposes and to improve the patient's quality of life. It can only be prescribed by a doctor after an accurately diagnosed examination and diagnosis. Independent attempts to remove warts are unacceptable, because patients without the necessary medical education and equipment cannot accurately determine the disease, and complications after such "treatment" occur more frequently than recovery.
There are several ways to treat warts. Everything is usually done under the supervision of a doctor, and some of it - only in the clinic treatment room.

Chemical Healing
Milk-salicylic colodion and salicylic patch is used to remove warts. Percentage of drug and method of use (long-term use of patches, application, etc. ) depends on the prevalence and localization of the neoplasm.
Zinc and 2-chloropropionic acid solutions can also be used. In this case, a chemical composition is applied to the previously treated surface, which is left on the wart until the color changes (depending on the type of wart). This procedure was repeated several times after 7, 14 and 21 days. Before each procedure, the tissue is removed mechanically.
Another chemical method is a combination of nitric, acetic, oxalic, lactic, and copper nitrate trihydrate acids. In this way, only relatively small neoplasms are treated - up to 5 mm. The solution is also allowed to change the color of the warts. After 3-5 days, the patient comes for a follow-up appointment, if necessary, he will be prescribed a second procedure in 1-4 weeks.

Cryodestruction
This method consists of freezing the wart with liquid nitrogen: a dampened tampon is pressed against the damaged skin (capturing several mm of surrounding tissue) for 1-5 minutes. Some lesions require multiple treatments four weeks apart to destroy them.
The main disadvantage of cryodestruction is its pain and delayed effect compared to other methods, where only one procedure is often sufficient for removal.
Electrocoagulation
Under the influence of an electric current, the warts are removed in layers. Such operations are performed under local anesthesia.
This method is more effective than cryodestruction, but has a significant disadvantage: electrocoagulation often leaves scars where the wart is removed. For patients who want to correct cosmetic defects, this method is not the most suitable.
this method is not the most suitable.
Laser destruction
Laser also removes warts in layers. The light guide hits the skin from a few seconds to three minutes, depending on its size. Then the scabs that appear are cut, and the lower part of the wound is laser treated again. The patient is then instructed on how to treat the wound. The operation itself is performed under local anesthesia.
Radio Wave Operation
Radio wave surgery is one of the most modern and gentle methods of removing multiple benign neoplasms, including warts.
This method is based on the generation of electromagnetic waves of different frequencies: from 100 kHz to 105 MHz. During the procedure, the tissue blocks the passing waves, which is why molecular energy is released inside the cells, which heats the skin. Under the influence of heat the cells completely evaporate - a neat cut is obtained. At the same time, no mechanical force is exerted on the affected tissue.
The advantage of this method:
- security;
- fast wound healing;
- good cosmetic effect - excluding scars and scars;
- is relatively painless - local anesthetic is applied before mini surgery;
- exclusion of secondary infection due to automatic disinfection of electrodes when the device is turned on.
The effectiveness of this method has been recognized worldwide, but it can be difficult to find a clinic that uses the radio wave surgery method.
Which maintenance method to choose
All of the above methods have some drawbacks:
- In the first few weeks, the operated area looks unattractive - crusts, dark tissue. This should be taken into account if the wart is on any visible part of the body (for example, on the face).
- Bad odor and some degree of pain during surgery.
In addition, each of these methods has contraindications, which you should be aware of at the initial consultation with a dermatologist.
But the main drawback is thatthere is a high chance ofrecurrence, especially if the warts are extensive, extensive. With each of these methods, doctors do not fight the root cause of the disease, but with the consequence, since todayhuman papillomavirus is incurable.
Therefore the therapy is directed at:
- or neoplasm damage that appears at the site of entry of the virus;
- is good for stimulating antiviral immune responses;
- or a combination of these approaches.
The most frequently used destructive treatment method. Efficiency reaches 50-80%.
Childhood is usually not a contraindication for surgical treatment. Hence, many of them (including radio wave surgery) are also used to treat warts in children. The exception is the chemical removal of warts due to possible adverse reactions to the material.
What to do after the
operationAfter one of these operations, be sure to follow your doctor's recommendations.
After removal of the tumor by one of the methods presented, the doctor usually prescribes the removal site treatment. It is forbidden to remove the "scale" on its own, wet the wound and expose it to direct sunlight.
If the patient continues to have warts, then he should consult an immunologist - possibly requiring drug therapy, which will increase immunity against the manifestations of the human papilloma virus.
Approx.
preventionIf the patient does not have immunodeficiency, the warts may disappear on their own, but this will take a long time - from several months to several years. So, in 65% of cases, warts reduce on their own within two years. If after two years the warts are still there, it is advisable to remove them. It is recommended to remove some growth immediately.
With normal immunity and a properly selected removal method (depending on the size and type of wart), pathogenic tissue can be removed and get a good cosmetic effect. With reduced immunity and other predisposing factors, human papilloma virus remaining in the body causes recurrence.
No specific disease prevention. But is infection inevitable?
You can reduce the chance of viruses if you follow a few rules:
- Avoid walking barefoot in public places where there is a possibility of skin injury and viral infection (swimming pool, public bathroom, gym).
- Choose quality footwear, replace it as often as possible. Try to keep your feet dry. Heat and humidity are excellent breeding grounds for human papillomavirus.
- To avoid periungual warts, visit a certified nail technician for a manicure and make sure they use sterile instruments.
For the prevention of anogenital warts, according to the WHO (World Health Organization), the quadrivalent vaccine against the human papillomavirus is also very effective. There is currently no vaccine available to prevent other types of warts.
If you find a single wart, don't try to burn, cut, or scrape it yourself - this way you can cause further inflammation and spread of the virus along the skin. After such "removal", instead of one wart in the morning, you can wake up with ten.














































































